601-608, Vedanta complex, Usmanpura, Ahmedabad – 13
601-608, Vedanta complex, Usmanpura, Ahmedabad – 13
The shoulder is the most moveable joint in your body. It helps you to lift your arm, to rotate it, and to reach up over your head. It is able to turn in many directions. This greater range of motion, however, can cause instability. Shoulder instability occurs when the head of the upper arm bone is forced out of the shoulder socket. This can happen as a result of a sudden injury or from overuse. Once a shoulder has dislocated, it is vulnerable to repeat episodes. When the shoulder is loose and slips out of place repeatedly, it is called chronic shoulder instability.
Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).The head, or ball, of your upper arm bone fits into a shallow socket in your shoulder blade. This socket is called the glenoid. Strong connective tissue, called the shoulder capsule, is the ligament system of the shoulder and keeps the head of the upper arm bone centered in the glenoid socket. This tissue covers the shoulder joint and attaches the upper end of the arm bone to the shoulder blade. Your shoulder also relies on strong tendons and muscles to keep your shoulder stable.
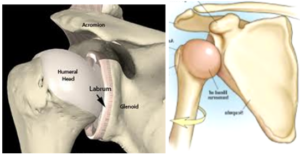
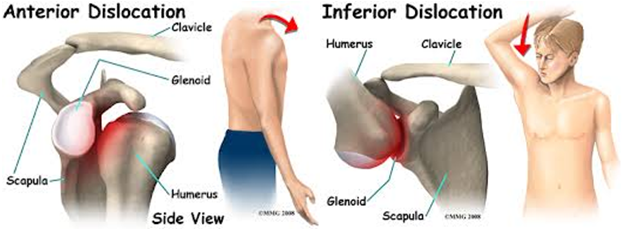
Shoulder dislocations can be partial, with the ball of the upper arm coming just partially out of the socket. This is called a subluxation. A complete dislocation means the ball comes all the way out of the socket. Once the ligaments, tendons, and muscles around the shoulder become loose or torn, dislocations can occur repeatedly. Chronic shoulder instability is the persistent inability of these tissues to keep the arm centered in the shoulder socket.
Severe injury, or trauma, is often the cause of an initial shoulder dislocation. When the head of the humerus dislocates, the socket bone (glenoid) and the ligaments in the front of the shoulder are often injured. The labrum — the cartilage rim around the edge of the glenoid — may also tear. This is commonly called a Bankart lesion. A severe first dislocation can lead to continued dislocations, giving out, or a feeling of instability.
Some people with shoulder instability have never had a dislocation. Most of these patients have looser ligaments in their shoulders. This increased looseness is sometimes just their normal anatomy. Sometimes, it is the result of repetitive overhead motion. Swimming, tennis, and volleyball are among the sports requiring repetitive overhead motion that can stretch out the shoulder ligaments. Many jobs also require repetitive overhead work. Looser ligaments can make it hard to maintain shoulder stability. Repetitive or stressful activities can challenge a weakened shoulder. This can result in a painful, unstable shoulder.
In a small minority of patients, the shoulder can become unstable without a history of injury or repetitive strain. In such patients, the shoulder may feel loose or dislocate in multiple directions, meaning the ball may dislocate out the front, out the back, or out the bottom of the shoulder. This is called multidirectional instability. These patients have naturally loose ligaments throughout the body and may be “double-jointed.”
Common symptoms of chronic shoulder instability include: Pain caused by shoulder injury Repeated shoulder dislocations Repeated instances of the shoulder giving out A persistent sensation of the shoulder feeling loose, slipping in and out of the joint, or just “hanging there”.
After discussing your symptoms and medical history, your doctor will examine your shoulder. Specific tests help your doctor assess instability in your shoulder. Your doctor may also test for general looseness in your ligaments. For example, you may be asked to try to touch your thumb to the underside of your forearm.
Doctor may order imaging tests to help confirm your diagnosis and identify any other problems. X-rays. These pictures will show any injuries to the bones that make up your shoulder joint.
This provides detailed images of soft tissues. It may help your doctor identify injuries to the ligaments and tendons surrounding your shoulder joint. The Bankart’s Lesion is the standard lesion associated with this condition. Some or other variant of this lesion may also be found if not standard lesion. The voluminous capsule is the other commonly associated finding with this condition.
This provides details of the bony structure of the shoulder. We are particularly interested in the Socket (Glenoid) shape and bone loss due to injury itself or the effect of rubbing (Erosions) in case of very frequent episode of the dislocation of shoulder. Bone loss on socket (Glenoid) side is important to decide about the possibility of the open bone augmentation procedures. The 3D CT also gives details of the depth of bone depression on the back side of the ball (Humerus Head) of shoulder in the form of Hill Sach’s lesions.
There is usually no form of the conservative treatment once the shoulder starts completely dislocating frequently but if its only first dislocation or there is only feeling of the ball about to come out of the socket without actual dislocation (Subluxation) conservative treatment of exercise in the form of the strengthening of the muscles of the rotator cuff and shoulder girdle could be tried. The exercise also helps in the certain borderline cases and habitual (Voluntary, Painless) dislocations.
Most young patients and those involved with any type of active sport are likely to need surgery to stabilize their unstable shoulder.
This is performed through 3 small holes (called portals). The Bankart repair involves re-attaching the detached capsulolabral complex to the glenoid using suture anchors. It is also possible to do a capsular shift (tightening of the lax capsule) at the same time. The advantage of the arthroscopic technique is its minimally invasive nature which minimizes morbidity of surgery and hospital stay. Further it allows excellent visualization of the entire shoulder joint and is very useful in detecting and treating other causes of dislocation like an ALPSA lesion as well as associated pathology like a SLAP lesion.
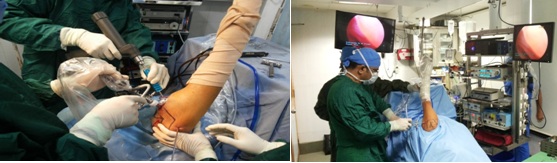
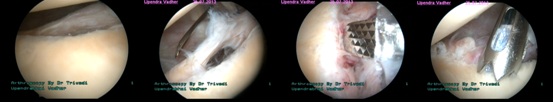
In cases where there is significant bone loss in the glenoid or a large Hill-Sachs lesion (engaging Hill-Sachs), a Bankart repair alone is likely to fail. In such situations a Latarjet procedure (transfer of coracoid process to the glenoid defect) or a bone graft to the Hill-Sachs lesion needs to be performed. These procedures require an open operation.
The patient may leave the hospital on the same day in case of an arthroscopic repair, and after 2 days after open surgery. The arm is placed in a shoulder immobilizer type of sling which restricts movement of the arm upwards, outwards and outward rotation of the arm. Depending upon the type of surgery performed and the strength of the repair achieved, the arm will be immobilized in the sling for a period of 3- 6 weeks. At around 2-3 weeks after surgery, pendulum exercises (gravity assisted movements of the arm) are initiated. At around 6 weeks after surgery, full range-of-motion exercises as well as shoulder strengthening exercises are started.
Overall it will take around 2-3 months after surgery for any patient to return to pre-operation status as far routine day-to-day activities are concerned. It may take around 3-4 months for a recreational athlete to return to sports, and even longer for a professional athlete (depending upon the nature of sport and the level of competition involved).